Although residents have no significant basic science research requirement, each resident is expected to complete one clinical, translational, or basic science research project per year to present at the annual James Barrett Brown Resident Research Day each June.
Optional research for a one- or two-year period with faculty members is available. Clinical research is represented across all the division’s Clinical Programs. As well, basic science research, including translational studies of novel therapies, are represented across our division within the Plastic Surgery Research Laboratories. “The Laboratories” encompass the basic and translational research within our division, which addresses major issues still faced by surgeons and operates within 8 themes that complement the Clinical Programs of our program – Aesthetics, Breast, Craniofacial, Nerve, Tissue Flaps, Tissue Engineering, Wounds, and Limb Transplant. A resident’s desire to do 1-2 years of research should be discussed prior to beginning training in the program. We strive for flexibility so residents are able to meet their personal career goals.
Faculty members’ research interest is summarized below:
Ida K. Fox, MD, has an interest in improving the function and lives of people living with cervical spinal cord injury. She has grant funding to look at outcomes after a relatively novel procedure — nerve transfer surgery to restore volitional control of hand and other upper extremity function. More recently she started a multi-site, multidisciplinary funded project to develop a decision support tool to help people considering nerve versus tendon transfer surgery in this setting. She is interested in factors that may help people make time-sensitive, individually unique and well-informed choices about their surgical care.
Susan Mackinnon, MD, has constantly evolving basic science, translational and clinical research occurring, primarily focused on peripheral nerve. In basic and translational research, Mackinnon has founded a basic science and translational research laboratory focused on peripheral nerve repair. In her basic and translational work, she uses animal models of peripheral nerve injury combined with surgical treatments to test prospective clinical advances. The work has led directly to changes in the clinical treatment of patients with peripheral nerve injury and to new understanding of nerve regeneration. Currently, her lab is focused on understanding the limits to reconstructing nerve gaps, where her work is supported by numerous grants including the NIH. In clinical research, she is interested in poorly described patient outcomes from peripheral nerve surgeries, with an aim to optimize surgical technique. Several of Mackinnon’s clinical research projects also involve bettering the occupational environment for surgeons. Since 2016, she has published in the fields of pregnancy during residency, residency preparation for surgical cases, and accidently injury in the OR. There is also a study underway to evaluate posture-related upper extremity pain in surgeons. Other clinical research involves an initiative on subclinical and clinical peroneal neuropathy, as well as a 3-tiered initiative to address the opioid epidemic.
Terence Myckatyn, MD, has research interests in clinical decision aids in breast reconstruction, outcomes of various interventions in breast reconstruction, and the development of enhanced recovery after surgery protocols. In addition, he is interested in the impact of biofilms on breast implants, their interaction with endogenous matrix proteins, and their potential association with capsular contracture and breast implant-associated anaplastic large cell lymphoma. In aesthetic surgery, he has research interests in optimizing satisfaction with breast augmentation and optimizing resident education. He also does research on the impact of inflammatory adipose-derived cytokines on metabolic disease. Dr. Myckatyn currently receives grant funding from the Siteman Cancer Center Investment Program, The Foundation for Barnes-Jewish Hospital, the Washington University Just-In-Time funding mechanism, the National Endowment for Plastic Surgery, the Aesthetic Surgery Education Research Foundation and several leading plastic surgery companies.
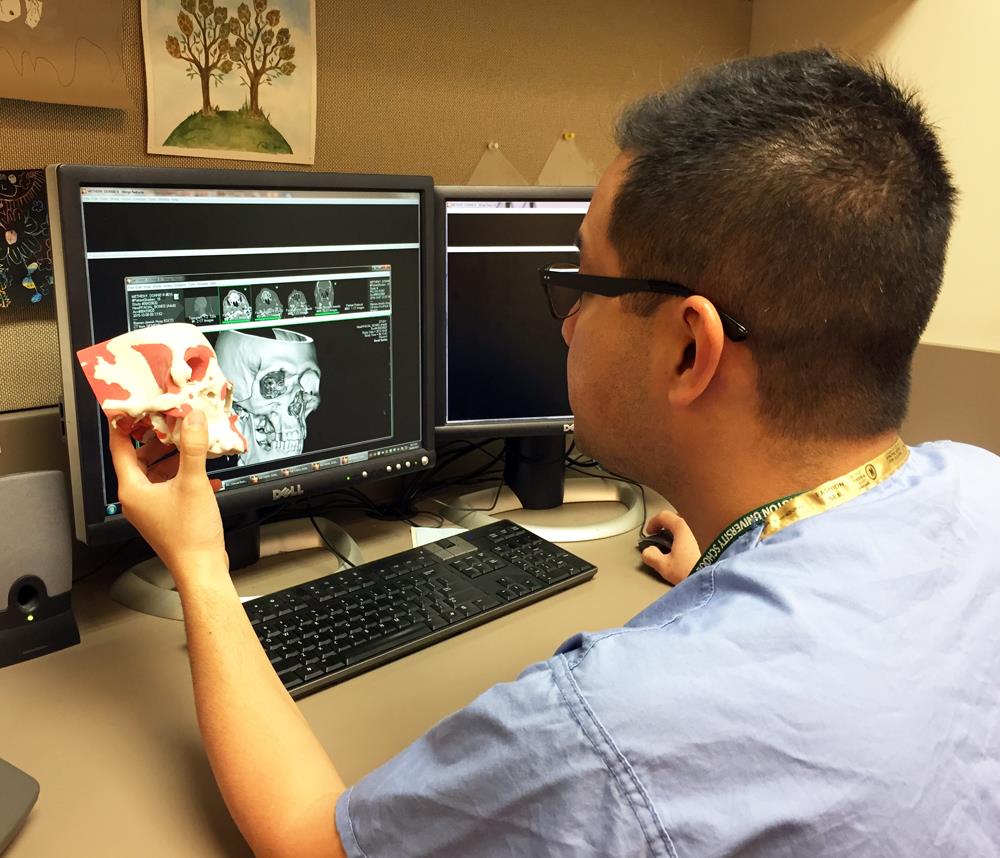
Kamlesh Patel, MD, MSc, research interests are to investigate clinical outcomes and optimization in delivery of care for patients with congenital (cleft and craniofacial) and traumatic anomalies. This work has allowed the transition to customized care for medically complex pediatric patients using a family/patient centered approach. His goal in performing research is to apply the results to decrease the rate of secondary procedures and treatment burden on patients and their families. More recently, he has created a multidisciplinary collaboration with Washington University’s Departments of Radiology and Neurosurgery to develop novel MR techniques to provide CT-equivalent 3D high-resolution cranial bone imaging. In 2017, Dr. Patel obtained a Master of Science in Clinical Investigation at Washington University to advance his ability to perform high quality clinical research. Through this program, faculty, residents and students have access to multiple resources to support clinical research.
Mitchell Pet, MD, has an interest collaborative interdisciplinary research aiming to bring technology and expertise in other fields into the realm of plastic surgery. By working with researchers in Washington University’s Departments of Anatomy and Neuroscience, Dr. Pet is working to introduce quantitative three dimensional modeling of complex articular surfaces for precision planning of reconstructive surgery. Additionally, through a new collaboration with engineers and materials scientists at Washington University and other institutions, Dr. Pet is working to develop and test the next generation of tissue perfusion sensors which will be useful for free flap monitoring and other applications across the reconstructive spectrum.
Justin Sacks, MD, our Chief of the Division of Plastic and Reconstructive Surgery, maintains a robust clinical, translational, and basic science research program with interests across many disciplines within plastic surgery, as well as a strong interest in entrepreneurship resulting from his studies. His basic and translational research involves interest in animal models of soft tissue reconstructions relevant to plastic surgery, as well as tissue engineering and 3D printing to reconstruct soft tissue injuries. From this experimental work, he has co-founded a number of start-up companies, including LifeSprout, that is creating state-of-the-art soft tissue scaffolds for reconstruction of the human form. Across his clinical research, he has conducted studies investigating many topics relevant to plastic surgery including aesthetic and breast reconstruction outcomes, tolerance strategies for vascularized composite allografts, vascular perfusion, and tissue flap reconstruction.
The lab of Alison Snyder-Warwick, MD, the Synaptic Glia and Neuromuscular Research Lab, has received funding for multiple projects by the NIH, The Plastic Surgery Foundation, and the American Association of Plastic Surgeons. Dr. Snyder-Warwick is currently completing her NIH Career Development Award (K08). The Snyder-Warwick lab investigates the interface between nerve and muscle, the neuromuscular junction (NMJ). Specifically, they focus on terminal Schwann cells, which are the specialized glial cells located at the NMJ. The lab investigates the roles of terminal Schwann cells during development, disease, muscular reinnervation and aging. Their goals are to identify the mechanisms of terminal Schwann cell function that may be manipulated into novel translational applications for clinical management of patients with peripheral nerve pathology. Dr. Snyder-Warwick also investigates clinical topics ranging from facial nerve-related challenges, women in plastic surgery, pediatric microsurgery, and care of children with cleft lip and/or palate.
Marissa Tenenbaum, MD, focuses on facial clinical outcomes in cosmetic surgery as well as breast reconstruction. Dr. Tenenbaum’s current projects include the impact of tumor to breast ratio on patient-reported outcomes following breast conservation therapy versus mastectomy with reconstruction. Others investigate the impact of simulation on patient-reported outcomes in breast augmentation and incision choice in nipple-sparing mastectomy in prospective, randomized control trials.
Thomas Tung, MD, has an interest in interdisciplinary research across plastic surgery, as well as a strong background to develop composite tissue transplantation. He previously developed animal models of limb transplantation to study the immunology of limb transplantation, nerve regeneration in the limb allograft, and the efficacy of costimulation blockade for the induction of tolerance.
Matthew Wood, PhD, is our Scientific Director of the Plastic Surgery Research Laboratories, where these Laboratories encompass the basic and translational research within our division. Wood’s group specifically investigates bioengineering approaches to advance the surgical management of peripheral nerve injuries and other soft tissue injuries. He is funded by an NIH R01 currently to study the role of T cells and other immune cells involved in nerve regeneration across nerve defects. His lab is also researching how electrical stimulation can be used as a therapeutic during surgery to improve the bodies endogenous abilities to regenerate. His work has been supported by grants from sources such as the NIH, DoD, Plastic Surgery Foundation, American Society for Surgery of the Hand, McDonnell Sciences Center, and the Hope Center for Neurological Disorders.